From time to time, Insurers can do a particularly good job of communicating a particular strategy or educating plan sponsors on a particular topic. This month (April 2016) Green Shield Canada came out with a very good document outlining their position and possibly that of their competitors with respect to the treatment of “generic” or more appropriately biosimilars or subsequent entry biologics. Please read on….
Introducing Green Shield Canada’s (GSC’s) Subsequent-Entry Biologic Policy
Subsequent-entry biologic drugs (or SEBs or biosimilars) are a hot topic in benefits circles as both plan sponsors and benefits providers consider the appropriate role they will play in the treatment process. At GSC we see SEBs playing a valuable role in our drug plans and have already developed a new SEB policy to guide our future decisions regarding these drugs. But, before explaining our policy, first we need to explain what SEBs are all about.
So… what’s a biologic?
Biologic drugs are currently one of the fastest growing areas in pharmaceutical development. These types of drugs provide treatment options for serious or rare illnesses where no effective treatments were previously available, such as cancer, rheumatoid arthritis, and multiple sclerosis. Increasingly, however, biologic drugs are also coming to market for many chronic diseases such as high cholesterol and asthma. Familiar drugs like vaccines and insulin are, in fact, also biologics. Here’s how biologics differ from traditional drugs.
| Traditional drugs | Biologic drugs |
| Produced through combining chemical ingredients | Produced using living microorganisms (e.g., bacteria) |
| Smaller, less complex molecules | Large, complicated molecules |
| Differences in manufacturing processes are unlikely to affect finished product | Even small changes in manufacturing process can affect the nature of the finished product and the way it works in the body |
While biologics are generally very effective in treating an increasing number of illnesses, they can be extremely expensive compared to traditional drugs.
So then, what’s an SEB? An SEB is a biologic product that is similar to an approved originator (or innovator) biologic product. Like all biologics, SEBs are complicated to develop and manufacture, and even small differences in production can make a difference in the way they work. Therefore, while they are similar to traditional generic drugs in that they are produced after the patent of the original biologic drug expires, they can’t technically be thought of as “generic biologics.” Unlike true generics, which are considered “bioequivalent” and therefore interchangeable with the brand-name drug, SEBs are not automatically interchangeable, and any new SEB that comes along is treated like a new drug.
GSC’s Subsequent Entry Biologics Policy
In developing our SEB policy, GSC undertook a comprehensive review and analysis of published information and evidence about the safety and efficacy of these drugs. In addition, information from European jurisdictions, many of which have had extensive real-world experience with the use of SEBs, was instrumental in crafting GSC’s SEB policy.
After considering this evidence as well the implications, and alternatives for covering SEBs, GSC has developed a unique approach: we are the first benefits provider to list SEBs as preferred products under our formularies. This means the originator products will be covered only in exceptional circumstances.
By not entering into any pricing agreements for originator biologics, GSC is able to leverage the cost savings available with SEBs while ensuring plan members have access to the biologic drugs they need.
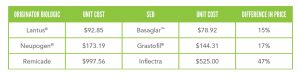
For example, Inflectra™ is the SEB for Remicade® (the originator biologic) – the drug with the highest volume of costs for GSC-administered health plans. We have listed Inflectra as the preferred product to treat rheumatoid arthritis, psoriatic arthritis, psoriasis, and ankylosing spondylitis. And recently we learned that we’re not the only ones to see the advantages of this approach. The provincial drug plans in Ontario, British Columbia, Alberta, and Yukon have also listed Inflectra as the first-line treatment for patients covered under a provincial drug plan. It is expected that remaining provincial governments will follow in the next few months.
In addition to listing Inflectra, GSC will be applying this same strategy to the other SEBs listed below, and when available later this year, we will include the SEBs for Enbrel and potentially Humira – the second and third highest cost-volume drugs at GSC – under our strategy.
A number of biologics will come off patent in the near future, so we expect to see more SEBs become available. With our new SEB policy, GSC is ideally positioned to take advantage of the current cost savings, future market forces, and competition that will continue to drive down the prices of SEBs, while at the same time ensuring plan members receive the most appropriate biologic drug for their condition.